Contact Us
YSCoBS - Your one stop solution for Medicare Advantage CoB
The Integrated YS Coordination of Benefits Solution revolutionizes Coordination of Benefits management in health insurance through a centralized, automated, and cloud-based system. It minimizes manual intervention by aggregating, verifying, reconciling, and resolving Coordination of Benefits data, enhancing efficiency and accuracy. The solution ensures scalability, security, and compliance while improving transparency and operational agility. By integrating external data sources, it enables seamless collaboration among stakeholders.
The system is designed to ensure scalability, security, and adaptability, enabling efficient management of extensive Coordination of Benefits data. By incorporating data feeds from various external sources, such as government agencies and insurance providers, it facilitates seamless communication and collaboration among stakeholders.
- Speeds Up Claim Processing
- Avoid hefty fines and penalties by CMS
- Improve first-pass claim payment
- Identify Coordination of Benefits errors
- Reduces Claim Denials
- Mention Compliance
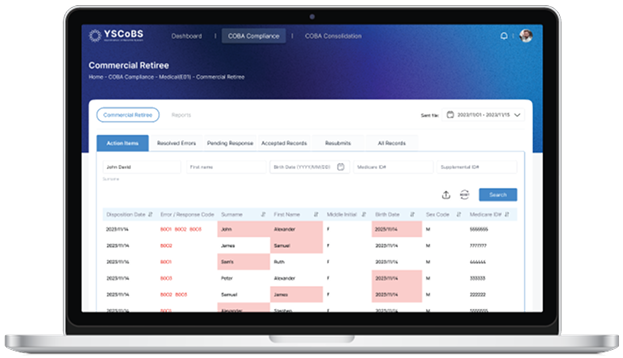
CoB Compliance
Become Compliance today
- Medical (E01)
- Pharmacy (E02)
- Medicare Secondary Payer (MSP)
E01 refers to the Electronic Coordination of Benefits claim submission format used for medical claims, part of HIPAA’s standardized EDI transactions.Key categories include

Commercial Retiree Plans
Speeds up claim resolution, reduces errors, and cuts administrative costs for both customers and insurers
Medicaid
Ensures timely, accurate claim processing, improving healthcare access for low-income beneficiaries
Medigap
Streamlines claims management, ensuring accurate billing and improving the customer experience by quickly addressing out-of-pocket expenses.
E02 (Pharmacy) is an electronic file format used for coordinating drug coverage information. Automating E02 file processing for drug coverage in Coordination of Benefits Agreement enhances coordination, reduces errors, and improves efficiency for timely updates and seamless claims involving:

Commercial Retiree Pharmacy Benefits
Drug coverage filing for Commercial Retirees speeds up prescription claims processing, reducing delays and improving access to medications.
Medigap Policies
Drug coverage filing for Medicaid beneficiaries accelerates claim processing, ensures accuracy, and improves access to essential medications.
Under Section 111 of MMSEA, mandatory reporting requirements for GHPs and NGHPs ensure accurate Coordination of Benefits and efficient Medicare claims processing. The goal is to:

- Ensure Medicare acts as a secondary payer where applicable.
- Reduce improper payments and improve benefit coordination.
- Verify beneficiary information and ensure timely reporting to avoid penalties.
CoB Consolidation
Coverage
Coordination of Benefits determines how health services and treatments covered by multiple insurance policies are coordinated, ensuring correct payment responsibilities between primary and secondary insurers.
Claim Errors
A HEDIS solution built to optimize member care
In today’s dynamic healthcare landscape, compliance with HEDIS (Healthcare Effectiveness Data and Information Set) measures is essential for payors aiming to enhance care quality, meet regulatory standards, and optimize performance metrics. Our HEDIS Improvement Solution is an all-encompassing platform that simplifies survey management, including Annual Wellness Visits (AWV), Health Risk Assessments (HRA), and Social Determinants of Health (SDOH) data collection.
Designed to streamline processes, this solution enables effortless data capture, automated reporting, and actionable insights via advanced dashboards. It empowers payors to close care gaps, engage members effectively, and deliver superior health outcomes—all while maintaining strict regulatory compliance.
Key Features (Must to know Essentials)
End-to-End Survey Management
Comprehensive support for surveys aligned with HEDIS, including AWV, HRA, and SDOH.
Customizable templates to address specific organizational and regulatory needs.

Advanced Reporting and Dashboards
Real-time compliance tracking with detailed performance analytics.
Visual dashboards monitor key indicators like care gap closures, member engagement, and demographic trends.

Seamless Systems Integration
Integrates seamlessly with leading Electronic Health Record (EHR) and Health Information Systems (HIS).
Ensures consistent data flow through API-driven architecture, reducing workflow disruptions.

Automation for Efficiency
Automates survey distribution, reminders, and data validation to reduce administrative burden.
Intelligent workflows ensure timely member assessments and follow-ups.

Data Integrity and Security
Ensures accuracy through robust data validation tools.
Adheres to stringent privacy and security standards, including HIPAA compliance.

Focus on Social Determinants of Health (SDOH)
Captures critical SDOH data to identify factors impacting healthcare outcomes.
Enables targeted interventions to address socioeconomic barriers to care.

- Why health plans love us
- Wellness Assessment
- AWV Checkup
- Youngsoft HRA/AWV Solutions
Elevated HEDIS Performance
Achieve higher compliance rates with streamlined data capture and reporting processes.
Enhance HEDIS scores to positively impact CMS Star Ratings and pay-for-performance programs.
Enhanced Member Engagement and Retention
Use real-time data insights to personalize outreach campaigns.
Build trust and satisfaction with proactive care gap closures.

Improved Operational Efficiency
Reduce administrative overhead through automation.
Optimize resource utilization and streamline workflows, resulting in cost savings.
Actionable Insights for Strategic Decisions
Leverage advanced analytics to understand member health trends.
Plan strategically with predictive insights into high-risk populations and emerging challenges.
Regulatory Compliance and Reporting Accuracy
Adhere to NCQA and CMS reporting requirements with robust tools.
Mitigate compliance risks with validated data capture and built-in audit trails.
Scalable and Future-Ready Technology
Scale effortlessly to accommodate additional surveys and analytics requirements.
Stay ahead of regulatory and industry trends with regular updates.
The HRA evaluates individuals’ potential health risks by analyzing personal health behaviors, medical history, genetics, and environmental factors. Data is collected through questionnaires, interviews, or physical exams and analyzed to assess risks for conditions such as cardiovascular disease, diabetes, and obesity.
Early Detection and Prevention
Identifies health risks early, enabling preventive interventions.
Personalized Recommendations
Tailored advice to mitigate identified risks.

Informed Decision-Making
Empowers individuals and organizations to make evidence-based health decisions.
Cost Savings
Reduces expenses associated with treating preventable chronic diseases.
Employee Wellness Programs
Integrated into workplace initiatives to enhance workforce health and productivity.
Research and Public Health Trends
Valuable data for campaigns and long-term health improvements.
The AWV is a preventive care appointment covered by Medicare and some private insurers. It focuses on assessing overall health, reviewing medical history, and setting health goals to promote well-being.
Preventive Care Focus
Detects health issues early, enabling timely intervention.
Personalized Health Plans
Provides tailored care based on individual needs.
Accessibility
Covered by Medicare and other insurers, reducing financial barriers.
Empowered Health Management
Encourages patients to take proactive steps for better health.
This web-based solution simplifies managing and conducting HRAs and AWVs. Designed with scalability and flexibility in mind, it ensures seamless integration into healthcare operations, supporting 24/7 access and enabling robust reporting capabilities.
Dynamic Program Management
Create and manage diverse programs like HRA, AWV, Smoke Cessation, etc.
Patient Onboarding
Bulk import or individual addition of patients.
Provider Assignments
Assign and manage submissions for providers with review and attestation options.
Digital Forms
Customizable and generic forms tailored per program, with data saved for future analysis.
Secure Document Storage
Upload documents to an S3 bucket.
API Integration
Real-time or scheduled data integration with client databases.
Campaign Management
Run targeted campaigns via CRM.
QR Code Integration
Enables quick HRA completion via QR scanning.
Key Insights
- Serving ~250,000+ Medicare and medicaid members through this program.
- Supports 100,000+ Medicare and medicaid members concurrently.
- Produces data in 5944 file layout for streamlined HRA submission to MDHHS.
- Ensures secure, encrypted access for administrators and participants.